Can You Be Sure It’s Melanoma?
Every year, thousands of Australians undergo biopsies for suspicious skin lesions. But even with a microscope, making the correct diagnosis isn’t always straightforward. Pathologists – highly trained doctors – can still disagree about whether a mole is benign or a potentially deadly melanoma.
This educational page is part of a four-part series designed to help you better understand the challenges, limitations, and evolving science behind skin cancer diagnosis. If you or someone you know is having a mole removed or has recently received a diagnosis, this series will give you the tools to ask smart, evidence-based questions.
Across the campaign, we’ll explore:
- Section 1: Why pathologists often disagree – and how misdiagnosis happens.
- Section 2: How new genomic technologies are helping to clarify the grey zones.
- Section 3: Patient stories and insights from experts on the frontlines.
- Section 4: What you can do to protect yourself and ensure diagnostic certainty.
📋 Now available: Our science-backed Melanoma Diagnostic Confidence 5-question checklist [PDF] you can take to your doctor, designed to help you understand the confidence level behind any diagnosis of a melanocytic lesion.
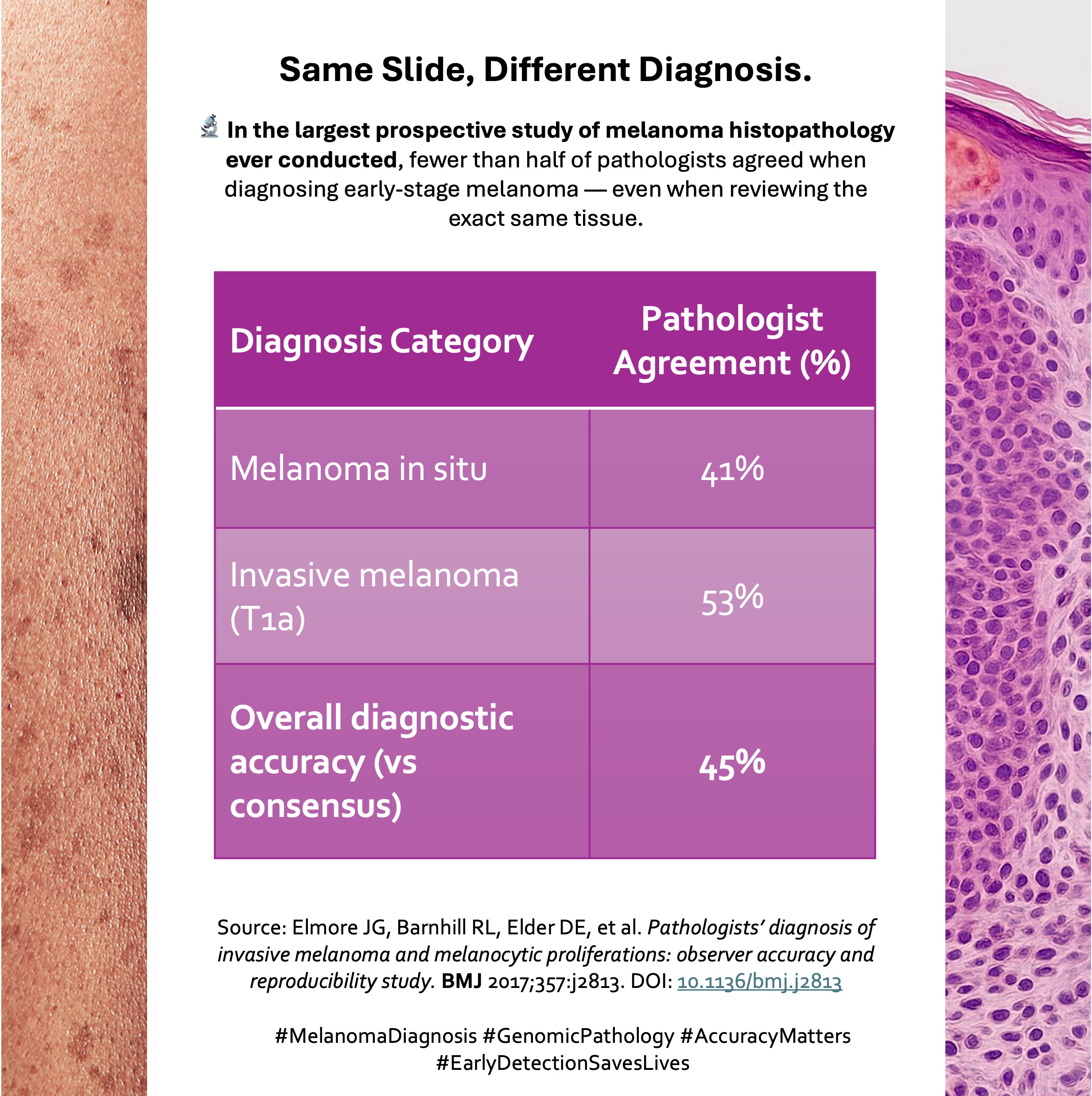
Diagnosing melanoma through histopathology has long been considered the gold standard, but even experts acknowledge that it can be imprecise. A 2017 study in BMJ revealed that when over 180 pathologists independently assessed the same melanocytic lesions, diagnostic agreement was surprisingly low: only 25% concordance for moderately atypical lesions, ~40% for melanoma in situ, and 43% for early invasive melanoma1.
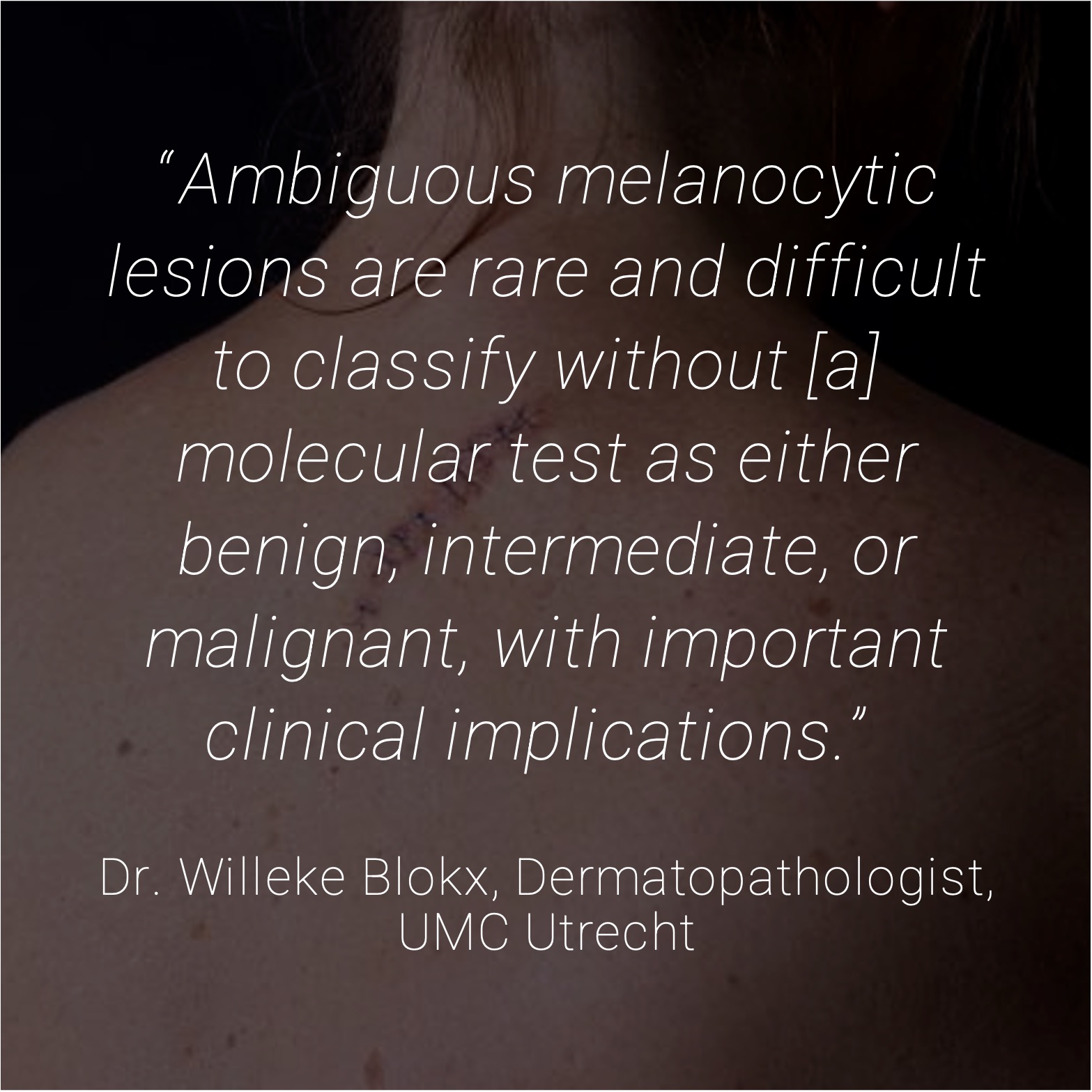
This variability isn’t due to lack of diagnostic effort – it’s a limitation of relying solely on visual interpretation. Histologic features often exist in a “gray zone,” where different specialists may see different things in the same slide. That’s why dermatopathology reports often include language like “borderline,” “indeterminate,” or “features concerning for melanoma but not diagnostic”1,2.
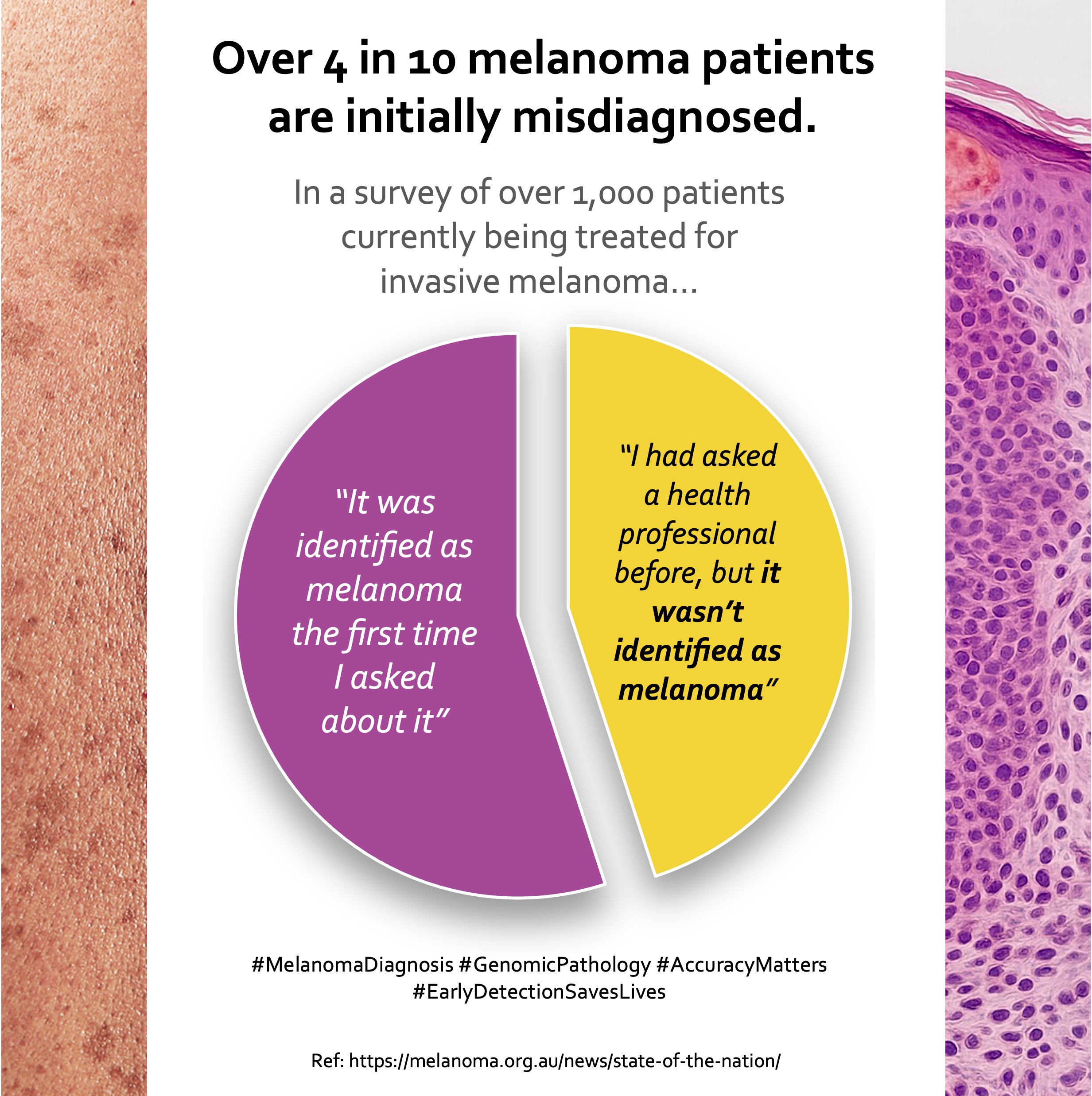
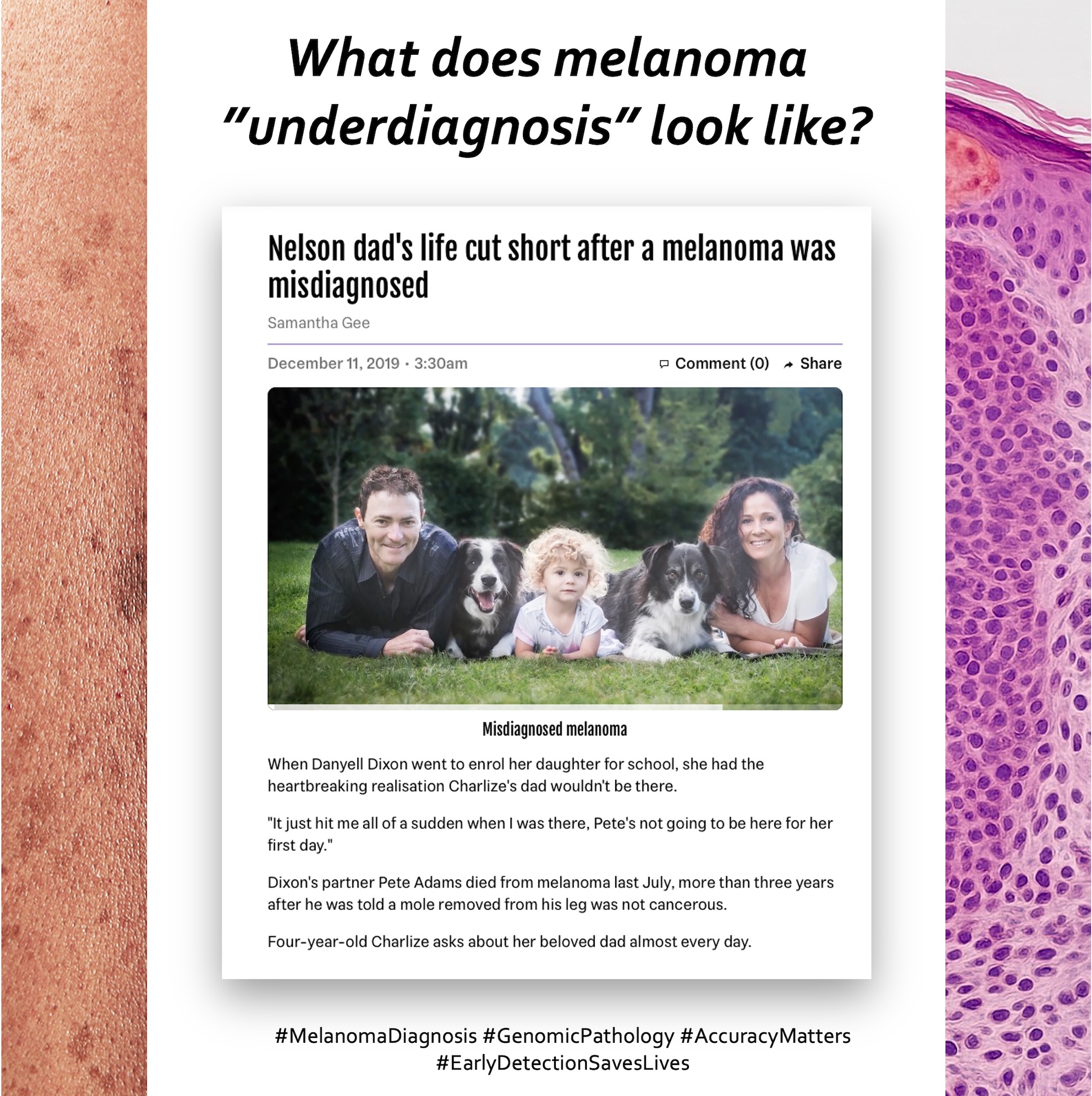
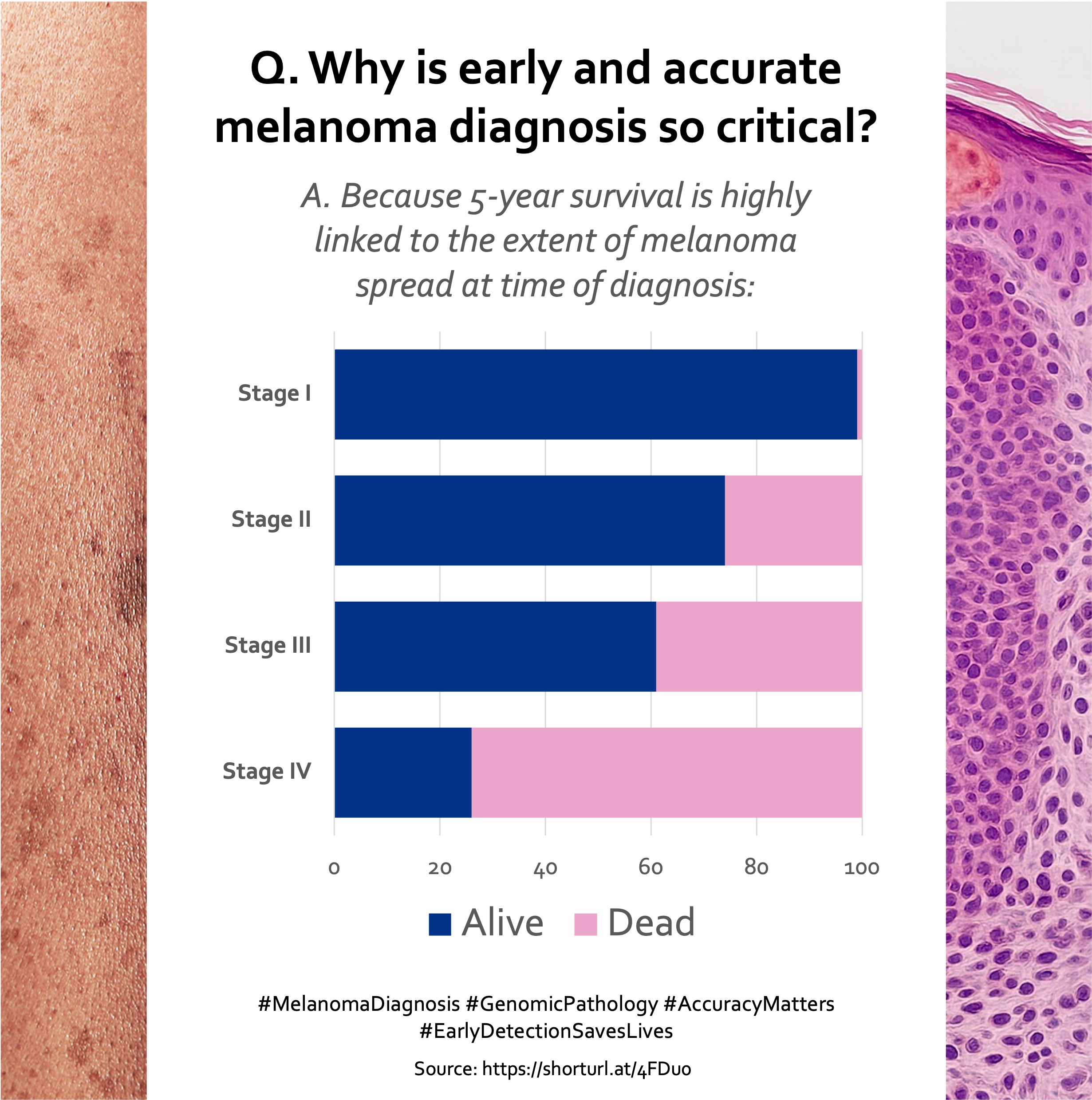
A broader meta-analysis suggests that as many as 40% of melanoma patients may be initially misdiagnosed, either receiving false reassurance or undergoing unnecessary surgery due to overcalling a benign lesion3. Misdiagnoses can lead to significant downstream effects:
- Under-diagnosis: Delayed treatment of actual melanoma, increased risk of metastasis
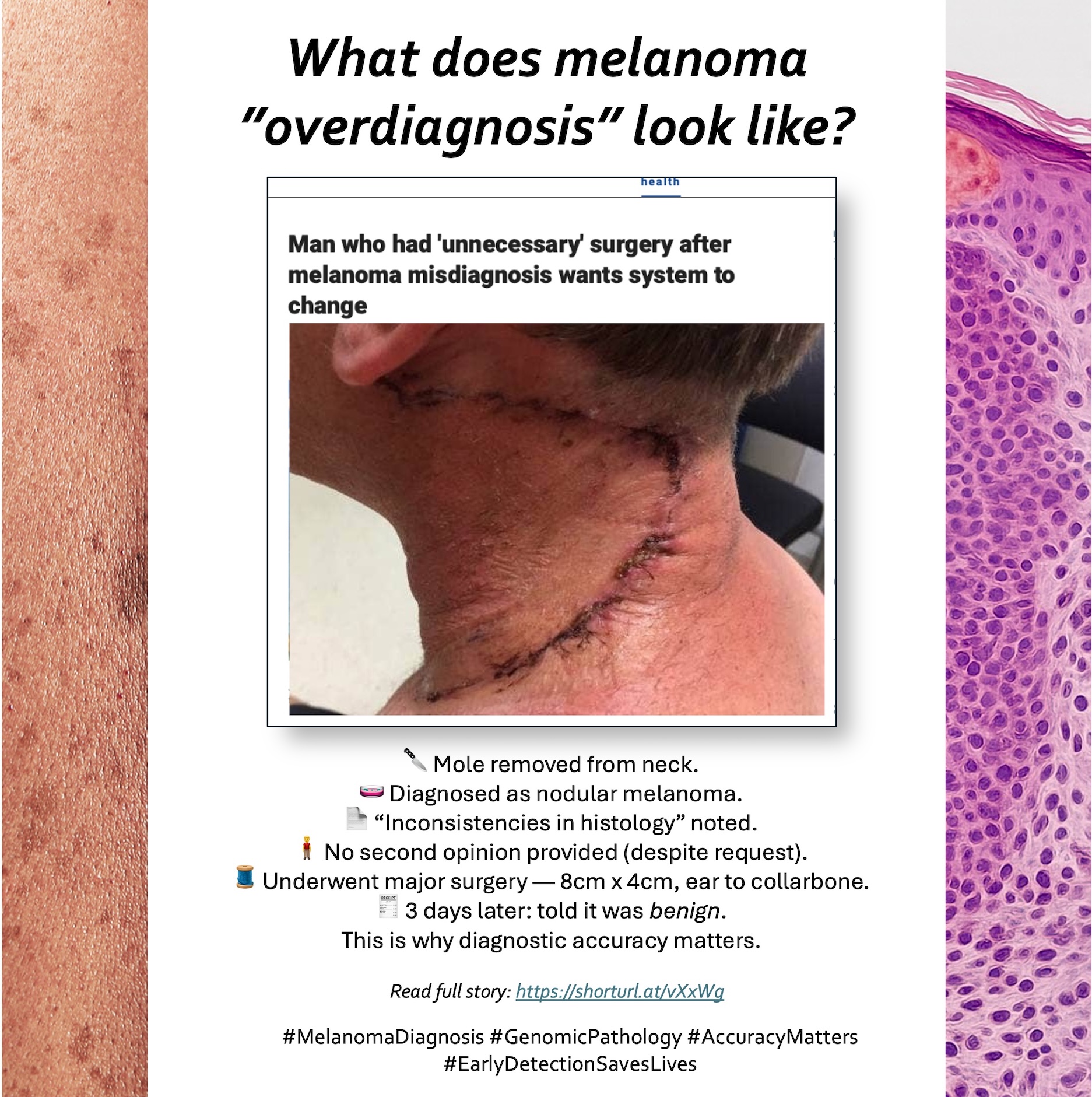
- Over-diagnosis: Unnecessary wide excision or sentinel node biopsy, patient anxiety, and overtreatment
Recognising these challenges is not a criticism of pathologists, it’s an acknowledgment of the complexity of early melanoma. This problem is now well-documented in the literature and supported by real-world clinical audits4. In this section, we aim to build awareness of this diagnostic uncertainty – the first step toward improving accuracy and patient outcomes.
Swipe through to explore diagnostic uncertainty →
References:
- Elmore J G, et al. Pathologists’ diagnosis of invasive melanoma and melanocytic proliferations: observer accuracy and reproducibility study BMJ 2017; 357 doi:10.1136/bmj.j2813.
- Melanoma Institute Australia & Melanoma Patients Australia. State of the Nation: A Report into Melanoma in Australia. 28 March 2022. https://melanoma.org.au/news/state-of-the-nation/
- National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015.
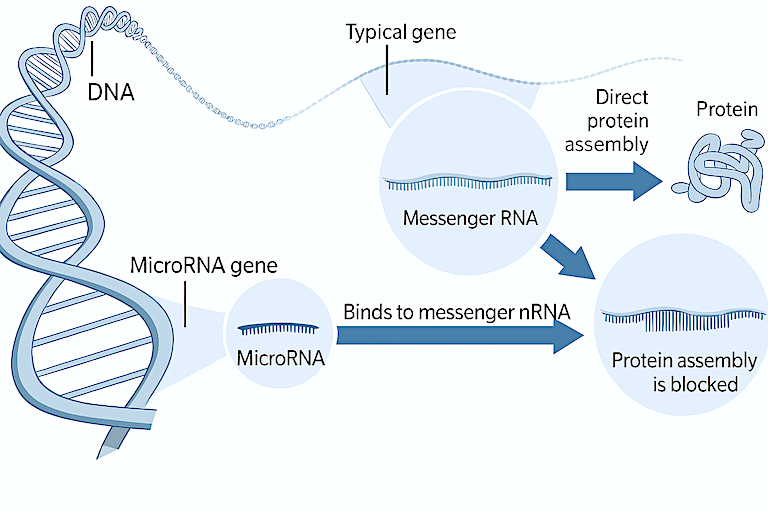
From DNA to RNA to Protein: MicroRNAs act like genetic brakes that bind to messenger RNA and can prevent certain proteins from being made. This hidden layer of regulation is now being used to better understand cancer behaviour.
When a mole is removed and sent to a pathology lab, the analysis typically involves a microscope. But now, scientists are also reading the genetic signals embedded within the tissue, a layer of molecular information that can reveal what even the most well-trained eye may not see.
Among these signals are microRNAs, tiny molecules that help control how skin cells grow, divide, or stop dividing. In melanoma, these molecules often behave abnormally. Some become overactive and drive cancer progression; others fall silent when they’re needed to suppress tumors.
Today, researchers can measure these molecular changes directly from the same biopsy block already taken for conventional diagnostic pathology. No extra procedure is needed, just a deeper read of the tissue you’ve already had removed.
These molecular patterns don’t rely on visual features alone. Instead, they reflect how the skin cells are functioning (or malfunctioning) on a genetic level. That means doctors may soon be able to classify uncertain lesions not just by what they look like, but by what they’re doing biologically.
Swipe to explore short videos →
References:
- Xu Y, et al. Differential expression of microRNAs during melanoma progression. Br J Cancer. 2012;106(3):553–61.
- Mueller DW, Bosserhoff AK. Role of miRNAs in the progression of malignant melanoma. Br J Cancer. 2009;101(4):551–6.
- Lou et al. miR-137 inhibits the invasion of melanoma cells through downregulation of multiple oncogenic target genes. J Invest Dermatol. 2013 Mar;133(3):768-775/li>
- Dror S, et al. Melanoma miRNA trafficking controls tumour primary niche formation. Nat Cell Biol. 2016;18(9):1006–17.
- Sand M, et al. MicroRNAs in non-melanoma skin cancer. Br J Dermatol. 2012;167(6):1146–51.
Diagnosing early melanoma is one of the most challenging tasks in dermatopathology. In this section, we present direct quotes from leading clinicians and researchers around the world, reflecting on the limitations of traditional histopathology and the real-world consequences of diagnostic uncertainty. These perspectives underscore why additional, objective tools are increasingly needed alongside expert opinion.
Swipe to explore stories →
Madison’s Story
Madison, a 28‑year‑old physician assistant, demonstrates how easily melanoma can be missed. As a teenager she had a suspicious mole on her forearm biopsied and was told it was benign. Years later a new mass on the same arm was also assumed to be non‑cancerous, so its removal was delayed. When the mass was finally excised, her doctors re‑examined the original pathology and found that the first lesion had actually been melanoma. Madison believes the misinterpretation allowed the tumour to spread, and she urges others to “listen to your body, seek multiple opinions and prioritise your well‑being.”
A Cautionary Tale from the United States
In 2015 a 42‑year‑old husband and father of three had a shave biopsy on a suspicious mole on his forearm. A dermatopathologist examined the tissue and wrongly reported it as benign. Three‑and‑a‑half years later he developed widespread disease; when cancer specialists reviewed the original slides they discovered the lesion was actually stage I melanoma. The delay allowed the cancer to progress to stage IV metastatic melanoma. He died within six months of diagnosis. This case, which resulted in a US$4.35 million malpractice settlement, highlights how a second histopathology opinion or adjunctive molecular testing might have changed the outcome.
Sarah Lee’s Story
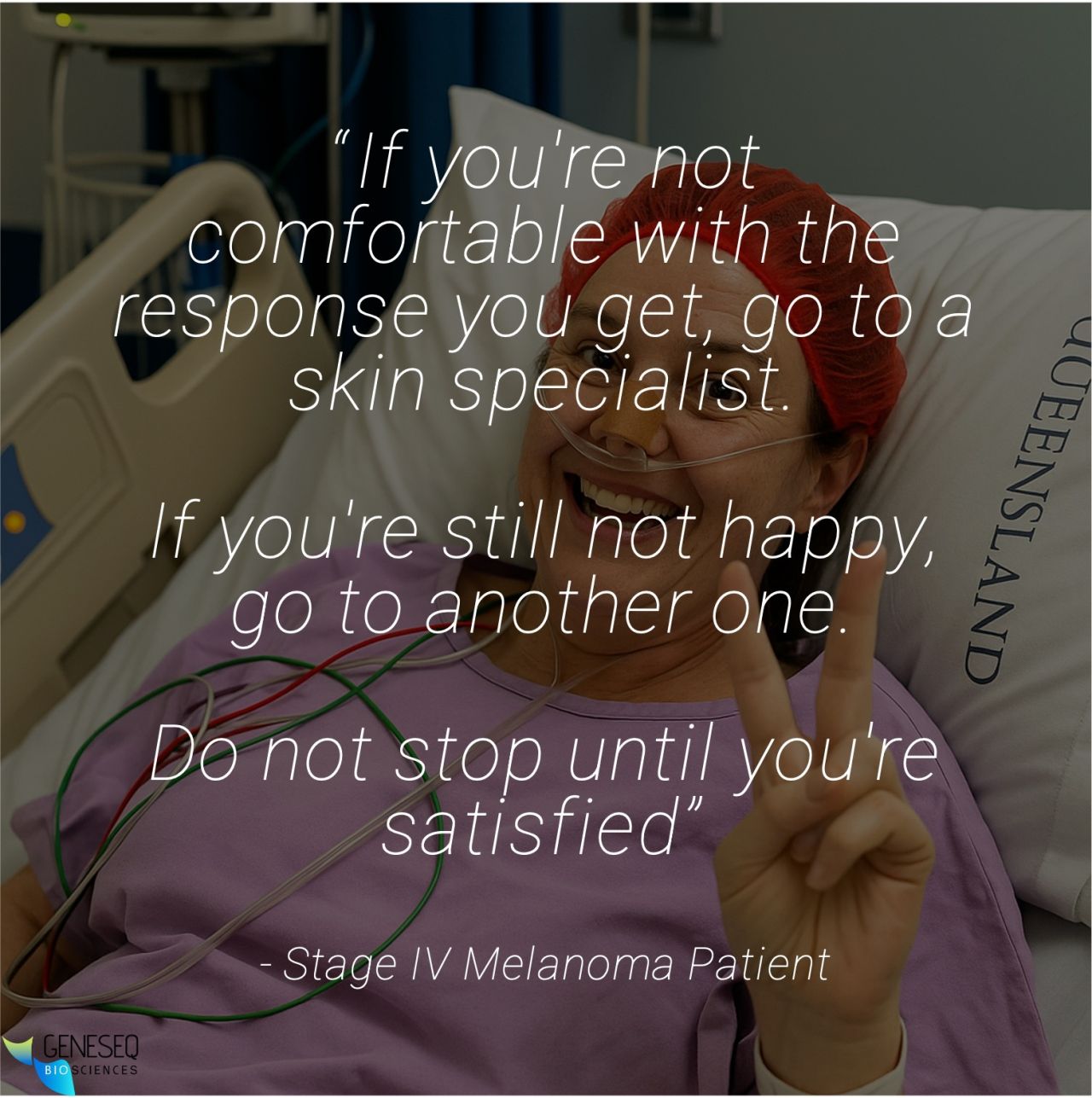
BBC journalist Sarah Lee shows how scalp melanoma can be misdiagnosed. After noticing a small dark lesion in her hairline, she consulted several doctors. One dermatologist said the spot “didn’t look unusual,” that she was “too young to have skin cancer,” and that scalp melanoma was almost impossible. Five months later the lesion had enlarged and her general practitioner thought it was a fungal infection. Unsatisfied, Lee sought another dermatologist, who immediately ordered a biopsy. The pathology confirmed stage III malignant melanoma requiring extensive lymph‑node surgery. She emphasises the importance of persistence when medical explanations do not match your instincts.

Bring this checklist to your next appointment.
This four‑part series has highlighted the challenge of diagnosing early melanoma, where even experienced pathologists may disagree, and the consequences of both delayed and over‑treatment are profound. In this final section, we focus on patient empowerment, providing practical steps and key questions that can help turn awareness into action.
Pathologists sometimes use terms like borderline, indeterminate, or concerning but not definitive when communicating the findings of their visual assessment of your biopsy tissue. Knowing how to respond to this uncertainty, by asking for a second opinion or additional testing, may help ensure you receive the most appropriate care for your individual situation, while also providing greater peace of mind.
Today, patients and doctors have access to new molecular tools that can look beyond the microscope and provide additional clarity using the same tissue already removed during your biopsy. These tests can help clarify whether a borderline lesion is truly worrisome or likely benign, supporting more confident decisions about surgery, monitoring, or further treatment.
✅ Take control: Ask these 5 questions at your next appointment
- Was my mole’s diagnosis clear or borderline? [Yes/No]
- Has my biopsy been reviewed by more than one pathologist? [Yes/No]
- Is there any uncertainty or indeterminate language in the pathology report? [Yes/No]
- Could additional molecular testing provide a clearer answer? [Yes/No]
- Can my existing biopsy tissue be used for a more in‑depth analysis? [Yes/No]
📋 Download the Melanoma Diagnostic Confidence Checklist (PDF)
Share this with your doctor to make informed, confident decisions.
References:
- Elmore J G, et al. Pathologists’ diagnosis of invasive melanoma and melanocytic proliferations: observer accuracy and reproducibility study British Medical Journal (BMJ) 2017; 357 https://www.bmj.com/content/357/bmj.j2813
- Australian Institute of Health and Welfare (2024) Cancer data in Australia. Australian Government, https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia.
- Melanoma Institute Australia & Melanoma Patients Australia. State of the Nation: A Report into Melanoma in Australia. 28 March 2022. https://melanoma.org.au/news/state-of-the-nation/